Mission minded
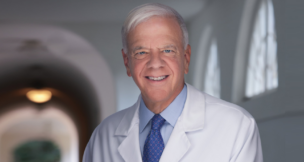
Transplant network CEO is drawn to complicated challenges
A Chicago woman with kidney failure was on a waiting list for 11 years because her body’s chemistry made it difficult to find the right match for a transplant. The Richmond-based United Network for Organ Sharing (UNOS), however, was able to locate the right kidney for her only a few weeks after a new allocation policy went into effect in December.
Brian Shepard, the CEO of UNOS, says the new system gives such difficult-to-match patients a better shot at finding the donated kidneys they need anywhere in the U.S. “For some of those folks, if they don’t get this kidney, the next one that matches them might be years from now,” he says.
Since 1984, UNOS, a private nonprofit organization, has managed the nation’s organ transplant system under contract with the federal government. With a workforce of about 330 people, UNOS handles the U.S. transplant waiting list, matching donors to recipients 24 hours a day, 365 days a year. About 123,000 patients need transplants annually, but only about 28,000 receive them. Nearly 80 transplants take place daily, but about 18 people waiting for transplants die each day.
Shepard became CEO of UNOS in late 2013 after serving as its chief operating officer and interim CEO. Before joining UNOS in 2010, he was director of policy under Gov. Tim Kaine (now a U.S. senator).
In deciding his next move when Kaine’s tenure ended, Shepard considered a number of options. “When I looked at them, I kind of realized they all had a public-service aspect — the work was meaningful — but they also had real intellectual, complicated challenges.”
Complicated challenges at UNOS include developing policies governing the allocation of donated organs after extensive deliberations. In addition to revising its policy on kidney transplants, which represent about 80 percent of all transplanted organs, UNOS is considering changes to its policy on liver transplants and is initiating rules for hand and face transplants, which remain relatively rare in the U.S.
While UNOS holds a contract with the federal government, the majority of its revenue comes from fees paid by transplant centers. In fiscal year 2013, for example, UNOS had revenue of $46 million, of which the federal contract represented $3.2 million, or nearly 7 percent.
April is National Donate Life Month, during which many events across the country are planned to focus on organ donations. In marking its 30 years of operation, UNOS is unveiling a new logo this month while collaborating with the Richmond-based Retail Merchants Association on an educational campaign and holding the inaugural United for UNOS 5K and Fun Run at Innsbrook in Glen Allen.
Away from UNOS’ headquarters, Shepard is an avid baseball fan who coaches his sons’ Little League teams. A long-range project has been taking the boys, ages 9 and 11, to all of the Major League Baseball parks during summer vacations. “We’re a little over half way through the list,” Shepard says.
A native of Roanoke, Shepard is a graduate of Virginia Tech who is now studying for an MBA at the University of Virginia’s Darden School of Business.
Virginia Business interviewed Shepard on Feb. 16 at his office in Richmond. The following is an edited transcript.
Virginia Business: How did UNOS wind up being in Richmond?
Shepard: The allocation system [for donated organs] … was a ground-up, a grass-roots effort. This really comes from the transplant community … Individual transplant centers would start to do transplants with donors that had come through their own hospitals. As technology evolved, people realized, if you put the kidney in a box of ice, you could probably get from VCU to Henrico Doctors’ [Hospital]. Then as the technology got better, they started to say, “We could get all the way to Washington, so I’ll call you if I can’t use the [donated organ], if you’ll call me when you can’t use it.” Individual, voluntary networks sort of grew up all over the country.
They started to get a little larger, and we ended up with multistate networks. By 1984, the federal government said, “Look … it’s time we had a single, national system.” The Democrats had control of the House, and the Republicans controlled the Senate at the time, and so the compromise was, “Yes, it’s going to be a government-mandated, national system, but it’s going to be run in the private sector, and we’re going to contract with somebody.”
It was the regional group based in Richmond called the Southeastern Organ Procurement Foundation that took the lead in calling other regional groups and saying, “Look, if somebody is going to do it, it ought to be us; it ought to be the transplant community. Let’s put together our own organization to bid for this contract.” We won that contract in 1984 and have held it through multiple rebids.
VB: When the contract comes up for rebid, do you have other competing bids?
Shepard: Other folks have bid before, [but] it’s difficult to find the collection of skill sets that we have developed in order to do the contract. We’ve got a very large IT team, but we’ve also got nurses in the site survey department that go out and check on hospitals. We’ve got a group of policy writers. We’ve got the 24/7 organ center. We’ve got a department full of biostatisticians. It’s hard for somebody to put all those pieces together.
VB: You’ve recently implemented a new policy on allocating kidney donations. How is it different from what was in place before?
Shepard: There are a couple of big differences … There are some folks who are just chemically very difficult to match [for transplanted organs]. If we can find a kidney that matches those folks, regardless of where it is in the country … the new system gives them even more priority. For some of those folks, if they don’t get this kidney, the next one that matches them might be years from now … In the first six weeks of using the system, [the new policy] seems to be delivering kidneys to those folks.
The other [change] is that we are attempting to give the kidneys that are likely to last the longest to the candidates who are likely to survive the longest. So the best 20 percent of kidneys are offered first to the 20 percent of candidates who are likely to live the longest based on medical data and their age and other things like that.

Shepard: Nationally, it’s probably around four years. And in some of the large, urban areas, it’s longer than that … There was a woman in Chicago … who had been waiting 11 years because she’s just almost impossible to find the right chemistry [in a donated kidney]. With the new system, we found one for her in just a few weeks. Some of that is luck, but she had a much bigger pool to draw from. It was not a local kidney that matched up.
VB: You are about to embark on a new branding effort. What’s your goal there?
Shepard: This is mostly about our communication with the transplant community. And it’s to tell the transplant community … we are building on 30 years of history here, and so it’s not a complete overhaul from what we used to look like, but we’re not exactly the same as we have been. There are some things we’re going to do differently moving forward from here. …
We’ll keep tuning up the allocation system. We’ll keep watching out for patient safety. But we’re really putting an increased emphasis on how the community works with our system …
How should we deliver information? How do we get them what they need to make the decisions? How do we make sure they’re not wasting time and money in the hospital setting that should otherwise be spent on patients, just because our system is not adapted for a new way they do business? …
We’re making those adjustments to be connected to the transplant community in a way that I think will ultimately make them better able to take care of their patients.
VB: And by transplant community, we’re talking about transplant centers …
Shepard: Transplant centers, the docs who work there, the organ procurement organizations that go out and recover the organs, those folks.
VB: How about visibility as far as recruitment of employees?
Shepard: That is a big deal for us, especially right now as we’re looking for IT [people]. We’re a nonprofit, so we don’t have shareholders banging on us, but also we’re running the IT infrastructure that connects all the nations’ hospitals and matches donor organs and recipients. So it matters whether we can get the right people.
VB: Is that hard? You’re competing with major companies for IT people.
Shepard: Sure. We don’t compete with Capital One for market share, but we sure compete with them for IT staff. But I think our mission-driven focus really helps us. We’re salary and benefit competitive, but the mission really is what sets us apart. A lot of times we’re able to attract folks from other jobs that don’t give that sense of fulfillment that comes from working here.
VB: [UNOS is] talking about policies for hands and face transplants. Have there been any policies before? Is this something totally new?
Shepard: This is completely new. The federal government changed the regulation around transplants last July to clarify that these were, in fact, organs …
We have now some basic membership requirements. We have some basic tiebreaker rules in place if an organ were to be provided and two candidates were actually good fits for it. But at this stage, that doesn’t happen … we don’t have those kinds of volumes [for these types of transplants] going on in the United States. There are a dozen [face transplants] total, and maybe two dozen hand transplants in the history of the United States …
We want to make sure that we’re able to provide sort of enough infrastructure around [these transplants] so that it is safe and that it is fair … These are pretty exciting medical discoveries; we want to let that unfold.
VB: One of the things that we mentioned in the story a couple of years ago was that … the number of organs offered for transplants was relatively flat while the demand keeps rising. Is that still the case?
Shepard: It is. We’re actually in the middle of a strategic planning process now … We’re going to adopt the next three-year strategic plan starting in June … We really touch so many pieces of the puzzle [in the transplant community] that it’s time we took an active role in seeing what we can do to increase the number [of donations].
And as the infrastructure folks [in allocating organs], that might mean something different than just advocating for more donors. We can look at: Does the way that we measure performance outcomes cause some centers not to use organs on the margins because they’re afraid their overall score will go down? And if that’s true, can we change the metric? Can we make the offer system work faster so that if you do have an organ that’s hard to place, it’s not eight hours later, it’s only two hours later? … Can we provide education to transplant centers about the benefits of using organs donated by older donors?
We’re about to release a study on deceased donor potential that suggests that, given the demographic trends in the United States, the organic growth in donors [is] just not going to be there. If we want more donors, we will have to do something different. We can’t wait for that to come to us … So we’ll need to be looking at using older donors. We’ll need to be more creative in some of the stuff we’re doing if we want more organs to be transplanted.
VB: I’m told that in some countries like Spain and Belgium they have an opt-out system where it’s automatically assumed that you’re going to be a donor when you get your driver’s license … whereas it’s an opt-in system here. Is there any opportunity or possibility of going to a system like they have overseas?
Shepard: I doubt it, and I’m not sure that it would help. They have a different sort of cultural baseline to work from. There are 58 organ procurement organizations [OPOs] in the United States. They each have a territory, so they’re roughly the size of a state … Some of them perform better than Spain. Some of them perform worse. So really it’s about the underlying demographics. It’s about the way the [organ procurement organization] goes about doing its job. It’s about the people that live in the area. It’s not as simple as saying, “Well if everybody opted in …” because OPOs are regularly able to get families to consent to donation even if the [deceased] persons hadn’t clearly made that decision in their lifetime. So it’s not just the number that [do commit to donating organs] in advance. It’s helpful to do it in advance. It makes it easier on the family … But it’s not the only way to get through a process. It’s not a magic bullet. And it’s not something I anticipate the United States would do anytime soon.
VB: Now, one issue that has been advanced a couple of times is the idea of compensating donors or the family of donors. Is that in the same realm of “never going to happen”?
Shepard: I think it’s unlikely. I think it’s an emotional decision for people to make. I don’t think that people’s reasons to [donate organs] or not really revolve around a few dollars. I do think, particularly with living donors, that there are some efforts that have been useful and some more that we can do to make sure that [making a donation] doesn’t cost them money — from replacing their lost wages to making sure their health insurance covers [the procedure allowing a donation] to making sure they’re not paying for their own tests, follow-up tests or something like that … I do think there are probably some additional things that we could do in that area. We don’t do any of it directly, but the transplant community does. But I don’t think direct payments, particularly for deceased donors, are on the table in the near future.
VB: Do you think there will ever be a time that organs are bought and sold?
Shepard: If we ever got to incentives, I would think you would have a single national standard of some kind, and it would happen through the system. Because the idea of some people being able to bid more for an organ than other people is really contrary to the values of the entire system. I wouldn’t see anything like that happen. I think even a regulated system of incentives is unlikely. But I certainly don’t think sort of an open market is ever going to happen.
VB: Is there anything that we haven’t touched upon that you wanted to bring up?
Shepard: I think we’ve got 30 years’ worth of history, and it’s an exciting time because we’re figuring out how to honor that history while we creatively look to the future. And the folks here couldn’t be any better to work with. It’s just a fabulous team of people.