Making a difference
Engineering students manufacture protective gear for health systems
Sydney Lake //June 30, 2020//
Making a difference
Engineering students manufacture protective gear for health systems
Sydney Lake //June 30, 2020//
As health care systems raced to locate new sources of personal protective equipment during the first months of the COVID-19 pandemic, Virginia’s engineering schools stepped up with innovative plans for manufacturing in-demand PPE.
In Roanoke, where the number of COVID-19 cases has remained much lower than Northern, Eastern and Central Virginia, Carilion Clinic health care system asked Virginia Tech in mid-April to help create a stockpile of PPE in the event cases began to surge.
Tech faculty, students and staff designed, produced and tested PPE and ventilation equipment, led by Chris Williams, director of Tech’s College of
Engineering’s Design, Research and Education for Additive Manufacturing System (DREAMS) Lab.
The school is producing face masks, face shields and breathing devices — but each had to undergo extensive product design and testing before being used by frontline workers. As of mid-June, Tech had produced approximately 5,000 face shields for local hospitals and health centers.
“We’re all just trying to do our best to help how we can, and every little contribution helps toward a greater end product,” says Genevieve Gural, a Tech mechanical engineering master’s student.
In Northern Virginia, the region with the greatest numbers of COVID-19 cases, George Mason University engineering students volunteered to produce PPE for Inova Health System through an effort led by Karen Livingston, associate director of entrepreneurship programs for Mason’s Office of Entrepreneurship and Innovation.
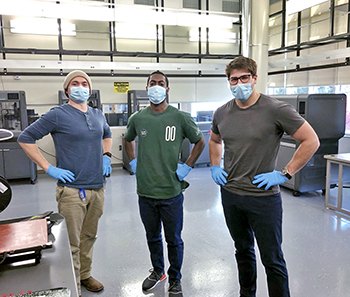
Mason engineering students who are also employees of the entrepreneurship office used 3D printers to make face shields and masks, which they engineered to be more comfortable for medical workers. They also created an attachable strap for masks that goes around the back of the head, instead of looping around the ears.
“Medical staff have been wearing these masks for long periods of time, and they hook behind the ears,” Livingston says. “It’s a really bad irritant.” As of mid-June, Mason engineers and entrepreneurship students had produced 12,000 such straps. (Some of her staff now include non-engineering students)
At the University of Virginia, engineers began 3D printing nasopharyngeal swabs, used for testing, in response to suggestions from health care workers.
William Guilford, assistant dean for undergraduate education and associate professor of biomedical engineering, started 3D printing the swabs after discussions with Dr. Taison Bell, a U.Va. assistant professor of medicine in Infectious Diseases and International Health and Pulmonary and Critical Care Medicine.
Although engineering faculty and staff are hard at work leading projects, students have been the backbone of design and production, says Alexander Leonessa, a Tech mechanical engineering professor who is leading a project that could produce up to 6,000 face shields for Blacksburg-area frontline workers.
“This has been a real-life experience of things we teach them in class,” he says. “It’s helped them grow as engineers, as team players and just people in general.”

from his apartment for Inova Health System. Photo courtesy George Mason University
3D homework
In order to promote social distancing, some students have made 3D printing projects into homework.
Liam Chapin, a Tech computer science student working on the face shields project, uses 3D printers in his own apartment to produce PPE. With his at-home printers, he can produce three face shields at once, but the process takes hours. The files he’s created, though, are posted to Tech’s public database and can be printed by anyone with 3D printer access.
However, “if something works somewhere else, it doesn’t mean it will work everywhere,” Chapin says. “We started out with designs that have been approved [and used] in other medical facilities … but were not suitable here because [hospitals] have different needs.”
Similarly, Mason has deployed a series of “3D printing farms” to produce PPE, three of which are located at the student employees’ homes.
“[When] we heard that we were going to have extended spring break and were uncertain of where we were going, we started creating 3D printing farms, taking our equipment elsewhere so we wouldn’t be putting any of our students at risk,” Livingston says.
Mason mechanical engineering student Dhawal Bhanderi manufactured reusable face shields from his family’s home in Virginia Beach while he finished his classes remotely.
“I can produce 20 quality shields a week,” Bhanderi said. “And while it may not sound like a great deal, the medical staff appreciate having this kind of personal protective equipment.”
Despite the spring semester wrapping up in May, the Mason engineering student employees will continue to print throughout the summer, Livingston says.
Supply chain challenges
As with most things COVID-19- related, working the supply chain to maintain supplies has been a challenge.
For the Mason face shield project, Livingston’s team changed the type of plastic it was using after supplies ran low.
“Sourcing materials has been interesting,” Livingston says.
Virginia Commonwealth University engineering professor Charles Cartin, who is working on a project to develop emergency ventilators with VCU Health, agrees that supply chain issues have “caused a lot more headache[s] than expected.” Some sources for PPE materials take only a couple days to ship supplies, while others can take weeks, he says.
Although Virginia universities are trying to keep up with demands for PPE, health professionals and the public have sometimes had to reuse medical grade masks or make their own from nonmedical fabrics. Health systems are also employing industrial decontamination and sterilization systems to reuse existing PPE.
Tech civil and environmental engineering professor Linsey Marr, who studies the airborne transmission of infectious disease, began testing the effectiveness of reusing N95 respirators and fabric masks in March.
Marr found that sterilized N95 respirators are effective for up to 10 uses after being sterilized, but homemade mask materials don’t fare as well. Microfiber cloth filters 80% of particles, while cotton and towel materials filter only 10% of particles.
Re-innovation
have been producing 3D-printed medical equipment for Sentara Healthcare.
In addition to making PPE from scratch, engineering schools are working with health systems to adapt existing medical equipment into in-demand ventilators needed to treat the most ill COVID-19 patients.
At Virginia Tech’s DREAMS Lab, Williams is in the early phases of working with Carilion’s chief pulmonologist to adapt cardiopulmonary bypass machines into basic respirators.
And in early March, Dr. Benjamin Nicholson, an EMS Fellow with VCU Health’s emergency department, approached Cartin, who is also the director of makerspaces for VCU Engineering, to develop a portable ventilator. Cartin and lab technician Adam Hamel developed a smaller ventilator that could be used in emergency settings using existing medical device attachments.

Cartin and Hamel are designing and developing the physical parts, such as paddles and levers, necessary to automate a manual respirator bag. The ventilators they’re designing are much smaller and more portable than standard ventilators, but the intent is to make them just as accurate and precise for emergency situations. As of early May, they had produced more than 15 prototypes of the portable ventilator, while seeking input from VCU Health.
“It was a little bit of back-and-forth learning,” Hamel says. “In the engineering department, we’re not doctors. Having input was very useful.”
Although the team is uncertain of an exact timeline due to U.S. Food & Drug Administration approvals, mass production is on the horizon.
“That’s part of Phase Two, where we’re going to look at other manufacturing processes to produce a large quantity,” Hamel says. “We’re not 100% sure [of the amount], but we’re planning to do mass production if everything goes accordingly.”
In Norfolk, Old Dominion University’s engineering school started producing 3D-printed medical equipment after being approached by Sentara Healthcare, which operates seven hospitals in Hampton Roads.
Dr. Jordan Asher, Sentara’s senior vice president and chief physician executive, asked Ben Stuart, interim dean of the ODU Batten College of Engineering and Technology, to collaborate with Sentara’s respiratory therapy program to design an adapter that would repurpose CPAP masks — typically used to treat sleep apnea — into viable PPE masks for health care workers.
Stuart enlisted Sebastian Bawab, professor and chair of ODU’s Department of Mechanical and Aerospace Engineering, and Tony Dean, associate professor and assistant dean for research, to lead the project. Justin Seemueller, a respiratory clinical specialist with Sentara, assisted the team.
At ODU’s Advanced Manufacturing Lab, which is equipped with industrial 3D printers, Bawab, Dean and a team of engineering students prototyped and produced adapters for the masks, delivering about 500 to Sentara hospitals by mid-May.
“We are still in production to have them on hand in case there is a second wave using the supplies obtained for this effort,” ODU spokesperson Sherry DiBari says.
Despite the vast effort it’s taken for engineering schools to mass produce PPE and prototype new ideas, it’s been well worth it.
“We’re filling a gap in the market,” Livingston says. “The pictures and texts that we get from the medical professionals on the front line … just remind us all of why we do it. They have all been so appreciative. Their days are so difficult now.”
Subscribe to Virginia Business.
i