Henrico County in contact with 39 of 41 nursing homes, fire chief says
After COVID-19 outbreak at care facility in county, emergency responders asked all centers what they need
Kate Andrews //April 3, 2020//
Henrico County in contact with 39 of 41 nursing homes, fire chief says
After COVID-19 outbreak at care facility in county, emergency responders asked all centers what they need
Kate Andrews //April 3, 2020//
After a news conference Thursday evening in which the Henrico County manager promised that county staff would be calling all of the county’s 41 nursing homes, the county Division of Fire employees followed through on the promise Friday.
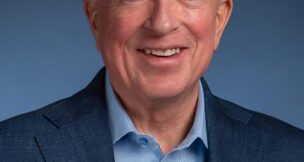
They spoke to employees at 39 facilities by mid-afternoon Friday, Fire Chief Alec Oughton said. As for the other two, “we’re sending a fire truck over there and asking them to answer their phone, please.”
In their contacts with the nursing homes, three said they were running low on personal protective equipment (PPE), which allowed the fire division to connect the centers with the Virginia Department of Health and the county’s Incident Management Team, a group of emergency responders from different departments in the county, which are helping the centers source more protective clothing, Oughton said.
The fire division has been closely involved with Canterbury Rehabilitation & Healthcare Center, where 17 residents ages 60 and older have died from conditions caused by COVID-19, and 108 people have tested positive. Early this week, the Henrico County Health Department assisted in testing all residents and staff members at Canterbury.
Although it has by far the highest number of confirmed cases, Canterbury is not the only nursing care facility in the region with a cluster of coronavirus cases.
A woman in her 90s who lived in the Masonic Home of Virginia in eastern Henrico died Friday, the county health department reported. Seven residents and one staff member at The Virginia Home near Maymont in Richmond have tested positive, Dr. Danny Avula, director of the Richmond and Henrico health departments, confirmed Friday. In all, seven facilities in the city and county have multiple cases, authorities said Thursday.
“These are really high-risk people in the community,” Oughton said. His division sent out an email to all 41 county nursing homes March 22 or 23 to notify them of changes in protocol in responding to emergencies after noticing a significant uptick in possible COVID-19 cases. One fire station responded to 19 calls at Canterbury that week, Oughton said.
Instead of sending five to eight EMTs and firefighters into a room for a 911 acute emergency call, as normal, the department now sends fewer people in to assess the situation — wearing full protective gear, including N95 face masks, Oughton said. If necessary, other responders will enter the room to help.
Sending in a smaller “recon crew” lets emergency responders conserve their protective wear and remain safer if they are dealing with a COVID-19 patient. Right now, 623 Division of Fire employees burn through between 60 and 100 N95 masks a day, Oughton said, but none have tested positive or had to be quarantined.
This is a lesson Oughton learned by reading a report the Kirkland, Washington, fire chief released to fire departments nationally while the city was ground zero for community spread of the virus in the United States several weeks ago. Oughton said he called the Kirkland chief to thank him for helping his division come up with an effective game plan.
Another thing that has changed is increased time after emergency calls, spent decontaminating vehicles each time a crew responds to a possible COVID-19 case, Oughton says.
But despite the obvious risk, firefighters and EMTs have signed up for extra shifts, and the number taking sick leave and annual leave is down, Oughton said. “I get a little bit emotional. We have an incredible work force. They will go out there and serve the community, and they don’t think about themselves.”
g