Providing hope
Virginia cancer centers offer array of advanced care

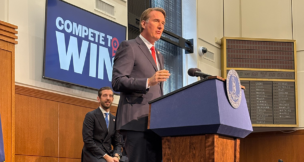
“There’s really no reason for anyone that is diagnosed with cancer in the commonwealth of Virginia to go out of state,” says Dr. Thomas Loughran, director of the University of Virginia Cancer Center. Photo by Caroline Martin

“There’s really no reason for anyone that is diagnosed with cancer in the commonwealth of Virginia to go out of state,” says Dr. Thomas Loughran, director of the University of Virginia Cancer Center. Photo by Caroline Martin
Providing hope
Virginia cancer centers offer array of advanced care
For cancer patients in Virginia, treatment options are growing. The state has two National Cancer Institute-designated comprehensive cancer centers, updated technology in clinics in Northern Virginia and the Shenandoah Valley, and soon, a larger treatment center in Roanoke.
The NCI reports that Virginians had a cancer incidence rate of 411 cases per 100,000 people from 2017 to 2021, below the national average of 444 cases, but digging into regional data shows geographical differences within the state. In Northern Virginia, incident rates were well below 400 per 100,000 people between 2016 to 2020, but in the Virginia Health Department’s Crater district, which includes Petersburg, Hopewell and Emporia, the incidence rate climbs to 515 cases. Mortality rates also are higher in Southern and Southwest Virginia compared with the rest of the state, according to the health department.
Although residents in larger population centers tend to have more options for medical care in general — including for cancer treatments — the expansion of cancer care facilities in Virginia means more people can access care, including ranges of specialties and treatment options.
Virginia’s multiple cancer centers are all part of larger health systems and offer advanced clinical care as well as supportive services for patients. Two centers conduct vast research as NCI comprehensive centers, while others focus more on consolidating care in one place for a patient to help minimize the burdens of finding and receiving varying treatments.
In 2022, the University of Virginia Cancer Center became the first institution in the state to be designated a comprehensive cancer center by the NCI. This means that U.Va.’s center receives funding from the NCI to provide advanced care to patients and conduct research. The Charlottesville facility employs 225 faculty researchers and 140 physicians.
In fiscal 2024, which ended in June, U.Va. Cancer Center saw 33,154 patients, up 10% from fiscal 2023. The center primarily serves residents from 87 counties, with about a third of patients living in rural areas.

“The bottom line is there’s really no reason for anyone that is diagnosed with cancer in the commonwealth of Virginia to go out of state,” says the center’s director, Dr. Thomas Loughran. “What distinguishes us from our community or colleagues is … the depth and breadth of faculty that are super-specialized in all these major particular types of cancers.”
One example of this specialization is the center’s high-risk pancreatic screening clinic, which monitors people with a family history of pancreatic cancer or who have pancreatic cysts.
One of the deadliest cancers, “pancreatic cancer is a really bad diagnosis, one of the worst, and [researchers] haven’t really made much progress in the last 20 years,” Loughran says. “The reason for that is it’s often detected at a time when it’s already grown quite a lot, because it doesn’t cause that many symptoms because of where it’s located.”
Patients in the high-risk clinic are carefully monitored, he says, and have better clinical outcomes. From 2013 to 2020, the five-year survival rate after surgery for clinic patients was 76%, compared with a 13% five-year survival rate for U.Va. patients who were diagnosed with pancreatic cancer but were not enrolled at the clinic.
Clinical advancements
U.Va. is also performing more treatments in an outpatient setting. The health system began offering chimeric antigen receptor (CAR) T-cell treatments at the Emily Couric Clinical Cancer Center in Charlottesville this year and is on track to have performed 52 by the end of the year. The treatment involves energizing T cells, which boost the body’s immune response, in a lab before infusing them back into a patient.
Virginia Commonwealth University’s Massey Comprehensive Cancer Center also offers CAR T-cell and bone marrow transplant therapies. In June 2023, Massey became the second center in the state to receive an NCI comprehensive cancer center designation. With about 500 doctors, the center treats patients who mostly hail from 66 localities across Central and Eastern Virginia, and saw almost 19,000 people last year, including 7,000 new patients.
Another highlight of VCU’s cancer treatments is its cardio-oncology team, a collaboration with the VCU Health Pauley Heart Center, which has specialists providing heart care to patients before, during and after cancer treatment. In 2023, the International Cardio-Oncology Society named VCU a center of excellence with gold status, its highest recognition.
VCU patients benefit from a multidisciplinary team approach between surgeons, medical oncologists and radiation oncologists, says Dr. Paula Fracasso, deputy director and senior adviser to the cancer service line at Massey. Additionally, the team works with other specialists, like cardio-oncologists, to address side effects.
“We do have a very good team of others who aren’t actually trained as medical oncologists or radiation oncologists to help us with side effects of treatment,” she says.
Directors of these and other cancer centers in the state say their technology or upcoming upgrades set them apart.
In Roanoke, Carilion Clinic‘s cancer facility opened in 1980, but a big expansion is on the horizon. In July, the health system announced it received a $25 million donation from former Advance Auto Parts CEO Nicholas Taubman and his wife, Jenny, to help build the new Carilion Taubman Cancer Center, which will be the hub of the health system’s oncology program. With approximately $70 million raised, Carilion expects to break ground on the estimated $100 million center this fall and open it in 2027.
“The Carilion Taubman Cancer Center will fill a major need to bring convenient, coordinated, collaborative and, above all, patient-centered cancer care to Southwest Virginia,” Lindsay Collins, vice president for Carilion’s department of medicine, said in a statement.
Technology for treatment
Meanwhile, U.Va. offers newer tech at its Focused Ultrasound Cancer Immunotherapy Center, which opened in 2022 as a partnership with the Charlottesville-based Focused Ultrasound Foundation. A noninvasive therapy, focused ultrasound uses ultrasound waves to target cancer locally and create a broader immune response in the patient’s body to a particular cancer.
In Northern Virginia, Inova Health System‘s Schar Cancer Institute provides inpatient and outpatient cancer care at its primary campus across the street from the Inova Fairfax Hospital, as well as at locations near its hospitals in Loudoun County and Alexandria and near another Fairfax hospital. Inova is also building a new Alexandria hospital on the former Landmark Mall site; it will include a new cancer center, says Dr. John Deeken, president of the Inova Schar Cancer Institute.
Inova’s cancer institute sees about 48,000 patients a year, of whom about 7,200 are new patients.
The institute also features a proton therapy machine, a type of particle accelerator that is about three stories tall. Proton radiation can better target cancer tumors and reduce damage to surrounding tissue.
“When we installed it five years ago, it was over $100 million for a machine, but it’s an important modality to offer to specific patients — pediatric patients, brain tumor patients, head and neck patients, some others — to better treat them compared to using the older technology,” Deeken says.
In Hampton Roads, the Hampton University Proton Cancer Institute, open for more than a decade, was the eighth proton therapy center in the nation. It focuses on providing care for prostate, breast, brain and spine cancers, as well as other cancers.
Also providing care in the region, Hampton Roads-based health system Sentara Health has three primary cancer centers in the state — the Sentara Brock Cancer Center in Norfolk; the Sentara RMH Hahn Cancer Center in Harrisonburg; and the Sentara Martha Jefferson Cancer Center in Charlottesville. Sentara handles direct patient care at the latter two locations, while Virginia Oncology Associates, Sentara Medical Group and Eastern Virginia Medical School, now part of the Macon & Joan Brock Virginia Health Sciences at Old Dominion University, partner to provide clinical care at the Brock cancer center. Both the Martha Jefferson and RMH centers see about 750 to 800 new cancer cases a year.
The Sentara RMH and Martha Jefferson centers each have two linear accelerators, a type of particle accelerator providing focused radiation treatments. The Harrisonburg facility is currently replacing one of its linear accelerators with a newer one, a roughly $4 million project.
Under the microscope
Cancer centers in Virginia also conduct research of varying breadth.
As NCI-designated comprehensive cancer centers, the U.Va. Cancer Center and VCU’s Massey center perform research in three areas: basic lab research focused on understanding cancer biology; clinical trials for new treatments; and population-based research studying the patterns and causes of cancer in population groups they serve.
U.Va. recently participated in a clinical trial for a new drug, tarlatamab, a targeted treatment for small-cell lung cancer. The drug latches onto tumor cells and T cells, which helps the T cell recognize and destroy the cancer cell. The Food and Drug Administration granted accelerated approval to the drug, developed by Amgen and branded as Imdelltra, in May.
“We were one of the first in the country to start treating patients on the FDA-approved medication, and as far as we know right now, we’re still the only institution in the mid-Atlantic region that is offering this to patients,” says Blake Herring, administrator for UVA Health‘s cancer service line.
In late August, U.Va. had treated 17 patients with the approved drug.
“It’s really turning some of these cancers into more chronic disease in a way, and managing it as, ‘You’re going to live with cancer,’ but keeping the cancer at bay,” Herring says. “To me, it’s remarkable just to be in oncology for over 18 years now and see how far we’ve come.”
At VCU’s Massey cancer center, doctors and scientists take a community-centered approach, aiming to communicate information about their research from studies in labs out into the community (and vice versa) and to patients’ bedsides, says Fracasso.
One example of this approach in action is work led by researchers Victoria Findlay, co-leader of the Cancer Prevention and Control Program at Massey, and David Turner, Findlay’s husband, looking at advanced glycation end products — certain proteins in food that are associated with chronic diseases and that are found in higher amounts in processed foods and foods cooked at higher temperatures, such as broiled or fried foods.
“They go to communities talking about nutrition and diet. Their laboratory benchwork is looking at prevention and more details about proving that they’re associated with cancer,” Fracasso says.
The Massey team also is proud of being a minority/underserved community site in the NCI’s Community Oncology Research Program, which requires a research site’s patient population consist of at least 30% racial and ethnic minorities or rural residents. About 40% of the patients in clinical trials led by Massey are minority patients, according to Fracasso, and Massey partners with 10 health systems and oncology medical practices for its trials.
“It’s to lead statewide clinical trials to foster research — clinical trials in minority and medically underserved patients. We have been awarded this for more than 30 years, and there’s only 14 MU-NCORPs in the country,” Fracasso explains.
Additional support
Although not a comprehensive cancer center, Inova’s cancer institute also participates in clinical trials research. Last year, the health system enrolled 983 patients in roughly 180 clinical studies, including 50 studies that were new that year.
“We’re really focused on how to better treat patients, so that’s why clinical research, as opposed to basic research, is where we focus on … and that’s what we really see as our sweet spot in terms of patient-directed research that really might benefit that patient, or at least patients in the near future,” Deeken says.
In the Richmond area, as of early September, Bon Secours was conducting 62 clinical trials across treatment trials, cancer symptom control studies, and research on how cancer care is delivered to the community.
In Hampton Roads, the Sentara Brock Cancer Center and other Sentara entities conduct research in partnership with Eastern Virginia Medical School and Virginia Oncology Associates. Dubbed the Luke Hillier Cancer Research Alliance, the collaboration was launched in November 2022 following a $3 million donation earlier that year from the Hillier Ignite Foundation. The alliance conducts clinical oncology research with a focus on health equities and outcomes.
These Virginia cancer centers also offer patient support services outside of clinical care, providing wraparound services. Most have dietitians, genetic counselors, social workers and financial counselors available, as well as psychosocial counseling and exercise classes. They also have nurse navigators, who guide patients from referral into treatment, answering questions and helping patients schedule initial appointments with physician teams.
Several Virginia cancer centers also offer additional therapeutic treatments, like acupuncture, massage and reiki. Sentara’s Brock center’s Carrillo Kern Center for Integrative Therapies houses these and other treatments, as well as a “healing garden” that includes art pieces.
“That was one of the things that we heard from a lot of our cancer survivors is that they kind of had to go out on their own to learn about complementary medicine,” says Meredith Strand, director of the Brock center. “It wasn’t something that was as strongly integrated as they’d like to see, and so we worked really closely with our providers and some small businesses in the community so we could offer truly integrated, whole-person care.”
In Harrisonburg, the Sentara RMH cancer center received a $1 million pledge, announced in August, from the Showalter family to expand its support services in the center, creating the Twila Showalter Supportive Care Clinic. Programmatic planning for the expansion is underway.
Much of Inova’s supportive services fall under its Life with Cancer program, which is being renamed the Peterson Life with Cancer program in recognition of a $15 million donation from the family behind Fairfax real estate developer Peterson Cos. More than 32,000 patients participated in the program last year.
Virginia’s cancer centers provide a wealth of options for patients, including relatively new treatments or clinical trials, while reducing the burden of scheduling appointments and otherwise managing care.
“It’s sad to see patients getting cancer,” Herring says, “but I think with the treatments and everything we’re doing, it makes me happy that we’re able to care for them, and [for] a lot of these patients that, before, there wasn’t a lot of hope. Now we’re providing more hope to them that they’re going to live.
s